Scientists are refining their understanding of neural networks and sharpening diagnoses.
By Vittoria D’Alessio
For two years, Dr Islem Rekik ran an EU-funded study to establish what the neural networks in a healthy brain looked like so that dysfunctional ones could become easier to spot.
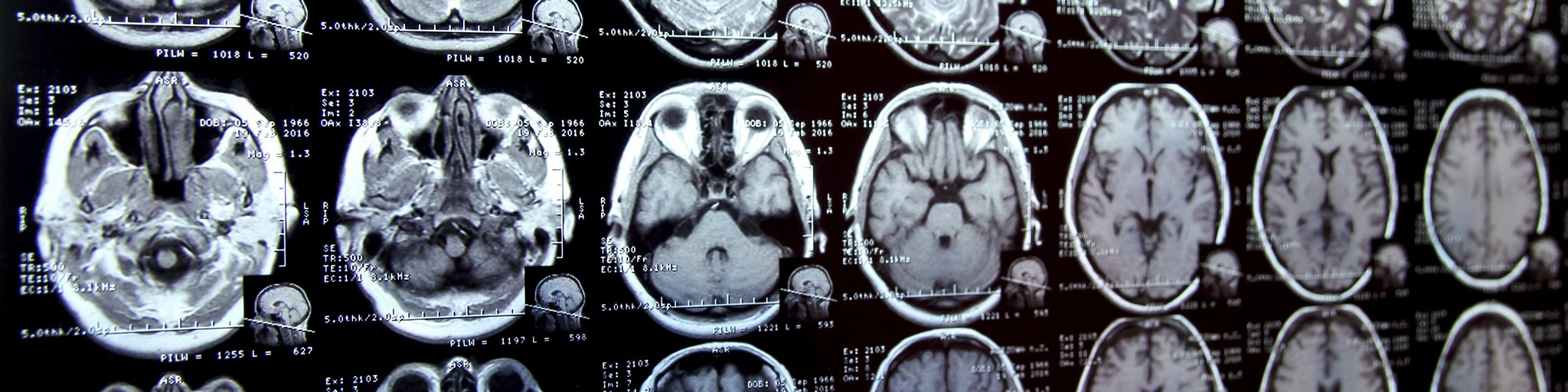
Rekik and her team took a large amount of data from 3D brain scans such as MRIs and turned these into 2D maps showing brain networks. Each network – known as a connectome and similar to an electric wiring diagram – revealed the labyrinthian system of neurons connecting the various zones of the brain.
Mapping the way
From these connectomes, the researchers produced brain connectivity templates, which act as neural fingerprints. These show how the brain is structured when all networks are arranged correctly and working as they should (while allowing for the natural variation expected in a given population of healthy individuals).
‘A disordered brain will show up as a map with networks that deviate from those seen in the healthy brain template,’ said Rekik, director of the Brain and Signal Research and Analysis laboratory, or BASIRA, at Istanbul Technical University in Turkey. ‘By placing such a map over the template, the dysfunction stands out.’
Brain disorders are an immense health challenge – both to the one in three Europeans expected to suffer from a neurological or psychiatric disorder and to the care services for victims.
Generally, the sooner these afflictions are diagnosed, the better. Early treatment heightens the chances of slowing or reversing potentially irreversible damage to brain tissue.
But some brain disorders, including Alzheimer’s disease, autism, epilepsy and sleep ailments, are particularly hard to diagnose. And even when these conditions are picked up, treatment options are often limited.
These kinds of diseases are categorised as ‘‘complex’’, reflecting the lack of a single fault in the structure of the brain or in the way it’s wired.
The challenge for scientists is not simply to identify the regions impacted by a complex brain disorder but also to pin down the tangle of neural pathways that are activated when messages are sent between affected regions.
Key connections
By better understanding these key connections, researchers can gain a more complete picture of complex disorders and begin the hunt for treatments to address the underlying network failures.
Rekik and her team produced their brain-network maps and connectivity templates in the NormNets project, which lasted for 24 months through March 2022.
The hope is that, by comparing the fingerprint of a disordered brain with that derived from a healthy brain population, it will be easier to spot faults in the network and – in time – direct a patient towards the most appropriate treatment.
The researchers are now refining machine-learning methods to analyse individual brain maps.
Eventually, they plan to make their healthy brain template open source. That means any expert working on diseases of the brain, from geneticists and epigeneticists to neuroscientists and neuropsychologists, will be able to use it freely in studies.
Using their mapping method, the researchers have already identified the top brain networks involved in mild cognitive impairment and certain forms of autism. Though preventative therapies and cures for these conditions are some way off, Rekik is convinced her group’s research will pave the way to future treatments.
‘The next step will be to design treatments that target not only a region of the brain but the entire connectome,’ she said. ‘The template will also be a tool to compare brain scans of individuals from cradle to grave, meaning we can track how the brain changes over time both in healthy individuals and in those who develop neurodegenerative disorders as they age.’
Advanced data
Another concern among scientists working on complex brain disorders is for people to receive a fast diagnosis so that personalised care can be delivered without delay.
The EU is funding a separate project to improve the diagnostic accuracy and clinical outcomes of complex brain disorders.
Called MES-CoBraD and running through March 2024, the initiative aims to develop a platform that can process diverse real-world medical data.
It collects and integrates large amounts of anonymised information from various sources including hospitals, existing research databases, smartwatches and fitness trackers.
This information is then used in the platform to conduct experiments that generate new scientific knowledge and to train computer algorithms supported by artificial intelligence (AI). The algorithms, known as Expert Systems, mimic and expand on the decision-making abilities of human experts.
Dr Christos Ntanos, research director at the Decision Support Systems Lab at the National Technical University of Athens in Greece, coordinates MES-CoBraD and stresses the promises and limitations of technology such as AI.
‘By introducing Expert Systems and artificial intelligence in neurology and in medicine in general, clinicians can multiply the positive impact they have on their patients,’ said Ntanos. ‘Though we must be careful – machines should be used to complement the expertise of medical professionals and help them make sound decisions. They’re not substitutes for human judgement and responsibility.’
By their very nature, complex brain disorders make a human-led diagnosis hard to come by. Often a disorder will show up with comorbidities, making it difficult to distinguish one affliction from another and clouding the diagnostic process.
‘Typically, even if the primary disorder can be diagnosed with relative ease, identifying the comorbid condition can pose a significant challenge,’ said Ntanos. ‘By using real-world data and advanced analytics and AI, we strive to improve diagnostic accuracy and identify the most effective treatments for both the primary condition and its comorbidity.’
Patient focus
MES-CoBradD plans to offer research institutes across Europe a platform for performing their own analyses and tests.
For instance, scientists from a university hospital can collect data from their own patients, anonymise the information, upload it to the platform and run experiments using the provided tools.
Doctors and their patients are also expected to benefit directly from the platform.
‘Eventually, the aim is for clinicians to use the platform’s Expert Systems to perform diagnoses on individual patients,’ said Ntanos.
He himself has been the subject of one of the project’s experiments.
‘I took part in a sleep study that used data collected in the past and data collected by volunteers like me in the present,’ Ntanos said. ‘When you don’t sleep very well – as I often don’t – a part of you wonders if it’s related to stress or something else.’
For a week, he kept track of meals and daily activities, answered lots of questions, took memory tests, wore a watch known as an actigraph that monitors rest-activity cycles and then got hooked up with 40 to 50 sensors before falling asleep.
‘The good news is that the platform and the neurologist agreed that there’s nothing neurologically wrong with me,’ Ntanos said. ‘It’s just stress.’
This article was originally published in Horizon, the EU Research and Innovation Magazine.