Professor Martijn Nawijn, an immunologist at the University of Groningen in the Netherlands, tells Horizon about his quest to map every cell in a healthy human lung. He says this work should help to understand more about the causes of lung disease – which is comparatively understudied – and should lead to new therapies in the next 15 to 20 years.
The lung is the largest surface area we have with the outside world. It’s very intimate, in the sense that it is a barrier to the outside, but it is really inside your body.
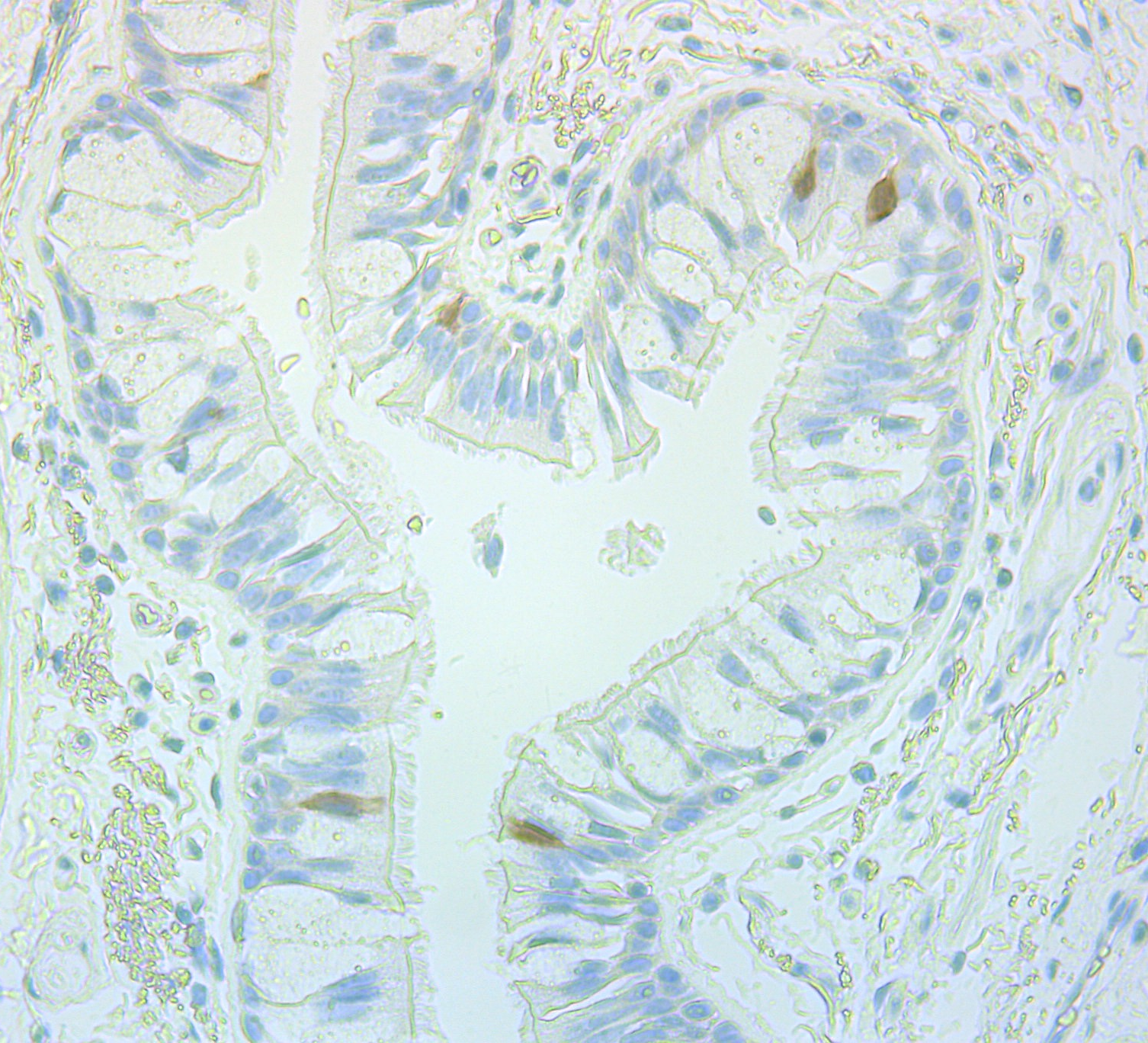
What we’re looking at in this picture is a piece of airway wall, where in the middle you see the lumen, the space where the air travels through. So that’s the outside world – that’s the air you inhale. The airways are the tubing of your lung, bringing the air from outside all the way into all the little alveoli (air sacs) where gas exchange occurs.
Most lung diseases are actually understudied. Some of them can be treated and you can suppress symptoms, but the underlying cause of the disease cannot be addressed at this moment. That’s strikingly different from some other diseases, where the progress over the last two or three decades has been much more pronounced, like cancer or cardiovascular disease, for instance. There’s a large unmet need to work on the lung and to understand how we could stop the process of disease progression.
My group, together with a lab in the Sanger Institute in England, a group from the Technical University of Munich and the Helmholtz Institute (in Germany), described the first ‘cell atlas’ of the human lung. That means we described what the cell type composition of the healthy human lung is. It’s the first time we’ve ever had a systematic description of the cell types that are in the human lung.
You can basically be healthy in one way, but you can be diseased in a lot of different ways. Once we know how the healthy situation is being maintained, we’re comparing that to how it is different in disease.

The edge of the airway wall is the epithelial layer, which sits on a basement membrane. To the right in the image, you can see the membrane quite well where there are these two lines in parallel. Then beneath it are the structural cells of the airway wall with fibroblasts (cells responsible for tissue structure), some smooth muscle cells, and there are immune cells as well that contribute to the surveillance of the airway wall to see whether there any infections. You can also see some red blood cells that sit in the small vessels that provide the airway wall itself with oxygen.
In this particular image, we stained for FOXI1, which is a protein that is a marker for a novel cell type called ionocytes. For instance, to the left in the image, there’s one brown stained cell a little bit towards the bottom. It looks very similar to the cells sitting next to it. Apart from the fact that we stained it to give it colour, you can’t really distinguish it.
‘There’s a large unmet need to work on the lung and to understand how we could stop the process of disease progression.’
-Prof. Martijn Nawijn, University of Groningen, the Netherlands
The ionocytes were discovered by two research groups independently (in 2018, using a new technique called single-cell RNA sequencing). The interesting thing about these ionocytes is that they are the cell type that expresses CFTR very highly. CFTR is the gene that is mutated in cystic fibrosis. It’s incredible that there’s this disease that people have been studying for 30 years, where there is this one gene that is affected, then there’s this cell type that really highly expresses this gene and we just didn’t know (it was there). It was almost by chance, using this novel technique, that they identified the cell type.
What we’ve been doing for the last 10 years (to research gene expression in the lungs) is that you take biopsies from the airway wall; you just basically take a bit of tissue, like you see in this image. Then you isolate the RNA (which carries genetic instructions from DNA) and you compare gene expression profiles between healthy and diseased tissue. Then you could see that some genes are more highly expressed in diseased tissue. Like mucus genes in asthma, for instance, because there’s much more mucus production than in healthy controls, so you will pick up mucus genes as being increased.
The problem with that technique is that if you take a biopsy, as you can see here, the biopsy contains at least 30 different cell types. The results are based on the average gene expression level for all cells.
Single-cell RNA sequencing takes the biopsy apart into individual cell types. Then for each cell, you look at the RNA and that allows you to quantify the composition of your biopsy by cell type.
It helps you to chart the composition of your tissue, but also it allows you to then see how the cells are different in diseased versus healthy. That is so much added information compared to what we used to do and that will really accelerate our understanding of disease.
I think the discovAIR project (to detail all the cell types in the lung in a cell atlas) is the outcome of a shift we’ve been making over the last three to five years. I was trained as an immunologist and made mouse models (to replicate human diseases). There’s not a single mouse experiment in the whole discovAIR project. So we’ve shifted from doing all this work in the model systems to using primary materials from patients and healthy donors.
In a few years from now, once we know in patients how the cellular composition is different between disease and healthy, we then need to look back again at the mouse models to see whether they actually accurately model this. So far, we have not been able to do that.
In discovAIR we will include many more regions of the lung, a wide range of ages and many more different diseases as well.
Meanwhile, we will also be improving the experimental mouse models and ideally working towards precision medicine interventions. This is where we know exactly how the disease has arisen in different patient groups, test whether a specific intervention works in optimised model systems, and then go back to the patient again. I think that in, say, 15 to 20 years, we’ll generate quite a few novel therapeutic approaches for lung diseases. It’s very exciting to be part of it.
As told to Ian Le Guillou.
This article has been edited and condensed for clarity.
The research in this article was funded by the EU. If you liked this article, please consider sharing it on social media.
Originally published on Horizon magazine.