Antibiotic resistant bacteria are killing more people each year, but scientists are turning to their natural virus predators to treat infections, as well as new vaccines to prevent disease.
In December 1945, during his Nobel Prize lecture for the discovery of penicillin, Dr Alexander Fleming warned that bacteria could become resistant to the drug if exposed to non-lethal amounts. ‘It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body,’ he said.
His warning proved prescient. Today, many bacteria are resistant to multiple antibiotics and therefore difficult to treat in patients. This happens because when you use antibiotics, bacteria evolve ways to flush out, sabotage or get around the effects of the drugs.
The consequences for human health are severe. Each year an estimated 700,000 people die due to bugs resistant to antibiotics. The World Health Organisation (WHO) predicts that this will reach 10 million deaths per year by 2050 if nothing changes.
To make matters worse, we are not developing new antibiotics fast enough. Of 43 antibiotics in development, none are novel drugs that adequately target a group of priority drug-resistant bacteria, according to a recent WHO review. In fact, no new class of antibiotic has been put on the market since the 1980s that tackles the most problematic bacteria, which are mostly in a group microbiologists call Gram negative.
‘The low-hanging fruit has already been picked. Now it is tougher and more difficult to discover new antibiotics,’ said Dr Guy-Charles Fanneau de la Horie, CEO of Pherecydes Pharma, a biotech company in France.
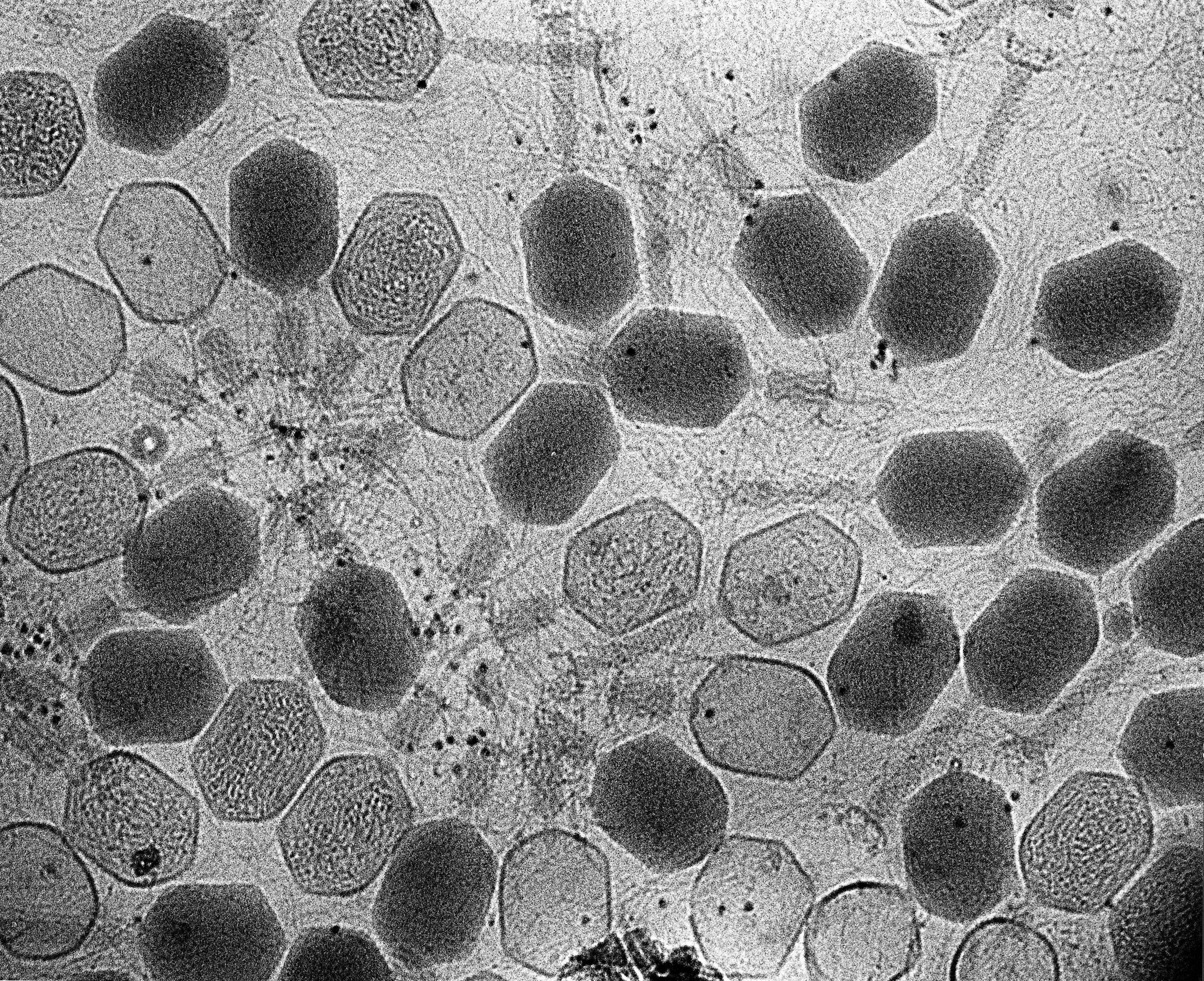
One alternative to finding new drugs is to make use of space-ship shaped viruses called bacteriophages (or phages) that prey on bacteria. Once phages land on bacteria, they inject them with DNA and replicate inside them. Soon, viral hoards burst out to infect more bacteria.
Germ-killing viruses
Dr de la Horie’s company, Pherecydes, focuses on manufacturing such phages and giving them to patients who are infected with drug-resistant bacteria. Its phages kill three species of bacteria notorious for resistance to frontline antibiotics – Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa. These are culprits for many drug-resistant infections in hospitals, where the most dangerous bugs reside, notes Dr de la Horie.
Injecting the phage viruses into patients should be perfectly safe because they do not target human cells. And unlike many antibiotics that impact lots of bacteria species, phages are more targeted and will not kill ‘friendly’ microbes in our gut. ‘They are highly specific,’ said Dr de la Horie. ‘For example, a phage that kills S. aureus will have no effect on Pseudomonas.’
As a more precise weapon, the correct phage must be chosen with care to kill the right bacteria. Consequently, Pherecydes has developed lab facilities to evaluate patient samples and to test the bacteria causing problems and choose a specific phage to kill them.
‘We discovered a small number of phages which we call super-phages, because they are active against a large number of strains within the same species,’ said Dr de la Horie. If a patient has Pseudomonas aeruginosa, a nasty bug often infecting patients on ventilators, then phages are administered that will kill more than 80% of strains.
Phage therapy is not yet authorised by the European Medicines Agency but Pherecydes has been treating patients with infections from drug-resistant bacteria after knee or hip surgery, through so-called ‘compassionate use’, where other treatment options have failed. These infections are especially difficult to treat with antibiotics. It is not a small problem. ‘Between 2% and 5% of joint replacements for hip and knee do get infected,’ explained Dr de la Horie.
So far, the company has used phages to treat more than 26 patients, mostly in the main hospital of Lyon, France. For example, reports show how it treated three elderly patients with S. aureus infection of knee replacements, as well as a patient with persistent Pseudomonas infection. There are plans to start up a trial for joint infections after hip and knee surgery later this year.
The company has also – with the support of a project called PhagoProd – developed sophisticated manufacturing processes for phages. Litre amounts are being made, but the plan is to scale this up to batches of tens of litres. Just one millilitre in a vial can contain 10 billion phages.
Even better, when phages are injected into a patient or applied to infected tissue, they multiply inside target bacteria, so that more of them are later available to kill bacteria. ‘Once you put the phages in the presence of bacteria, you should not need to put more in again, because they will multiply themselves,’ said Dr de la Horie.
Dr de la Horie hopes that a large patient trial can begin in 2023. ‘We believe our products could be on the market at the earliest by 2024, or maybe 2025,’ he said.
‘We discovered a small number of phages which we call super-phages, because they are active against a large number of strains within the same species.’
Dr Guy-Charles Fanneau de la Horie, CEO, Pherecydes Pharma
Prevention, not cure
One of the problem bugs – Pseudomonas aeruginosa – is among the targets of a project called BactiVax, which is also tackling the challenge of antibiotic-resistant infections. Rather than using phages or other methods to treat infections once they arise, however, the BactiVax researchers have their sights set on vaccines.
Pseudomonas plagues patients in intensive care, patients with chronic obstructive pulmonary disease (COPD), and patients with cystic fibrosis.
It can cause chronic infections as well as severe infections. ‘It is quite common, and is sometimes not really damaging,’ said Irene Jurado, doctoral candidate at University College Dublin in Ireland, ‘but it can be a problem for people with underlying conditions.’
If a child with cystic fibrosis is infected with some strains when they are 5 or 6 years old, the bug can stay in their lungs for their entire life and complicate their breathing and make them severely ill, she adds.
Pseudomonas has a large genome, which gives it plenty of flexibility to adapt to different challenges, something Jurado recently wrote about. This makes it especially skilled at developing resistance to antibiotics. Consequently, researchers tried for decades to develop vaccines against it, but without success.
Jurado is investigating the proteins that the bacteria uses to attach to lung cells. This could provide crucial components to a vaccine, in the same way as the SARS-CoV-2 spike protein in Covid-19 vaccines tutor our immune system.
‘We are trying to see what immune responses are needed to protect people from infection,’ explained Dr Siobhán McClean, an immunologist at University College Dublin, Ireland, who leads BactiVax. The proteins that bacteria use to stick to our cells are often good vaccine targets. For example, the whooping cough vaccine uses five different proteins that the bacteria hooks into cells that line our throat.
Unfortunately, the bacteria is a tougher foe than the Covid-19 virus, since it has not one, but dozens of proteins on its exterior. This means that what should go into a vaccine is less obvious with Pseudomonas, than for the pandemic virus, where the spike protein is the go-to target.
But researchers believe that a vaccine is worth the effort. ‘Our idea is that if we can get a vaccine to prevent infection, it’s better than constantly trying to treat (problem infections) with antibiotics,’ said Dr McClean. ‘We’re down to the antibiotics of last resort and when they run out, we’re going to be stuck.’
The research in this article was funded by the EU.
Originally published on Horizon Magazine